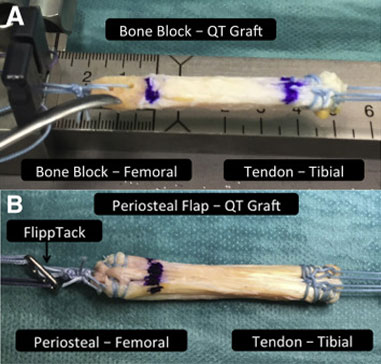
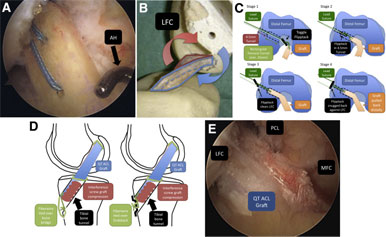
Fig 2
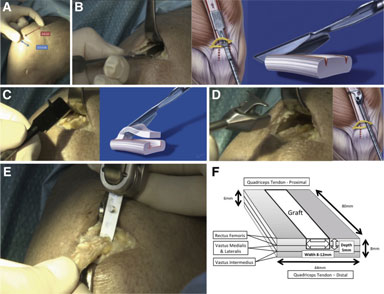
Quadriceps tendon (QT) graft harvesting. (A) The transverse skin incision for minimally invasive QT harvest is shown in a cadaveric right knee. By use of minimally invasive instrumentation, a QT graft 6 to 8 cm long (indicated by the surgeon and illustrated in red) and 8 to 12 mm wide can be harvested subcutaneously through a 2.5- to 3-cm transverse incision (shown in blue). (B) Double-knife insertion is shown in a cadaveric right knee viewed from medially and schematically. After exposure of the tendon, a double knife (Karl Storz) with a width of 8, 10, or 12 mm is inserted, starting at the middle of the superior patellar border, to a minimum depth of 75 mm (judged using calibrations on the instrument handle). (C) Tendon separator insertion is shown in a cadaveric right knee and schematically. The graft thickness is determined with a 5-mm tendon separator, which undercuts the QT as shown. The separator is inserted to the same length as the parallel bladed double knife (minimum of 75 mm) as determined by calibrations on the instrument handle. (D) Proximal tendon division and retrieval are shown in a cadaveric right knee and schematically. Both are accomplished using a specially developed tendon cutter–grasper (Karl Storz). Firm compression of the handle divides the tendon proximally subcutaneously. The tendon cutter is then closed around the tendon less sharply and used as a grasper to retrieve the tendon end. (E) Bone block harvesting is shown in a cadaveric right knee. After pre-scoring of the periosteum with a scalpel to outline the desired 15-mm-long by 8-, 9-, or 10-mm-wide and 5-mm-deep bone block, an oscillating saw is used for medial and lateral sagittal cuts, the distal transverse cut, and last, the final posterior coronal cut (illustrated in panel E). Use of an osteotome is recommended to give extra control in final block separation and to reduce the risk of patellar or bone block fracture. (F) The QT is a trilaminar structure formed from the confluence of the rectus femoris superficially, vastus lateralis and medialis in the middle layer, and vastus intermedius in the deepest layer. The laminae fuse with a degree of individual variation over a 13- to 90-mm region (mean, 44 mm) proximal to the superior pole of the patella.7 The width of the QT at the patellar insertion in adults is 44 mm on average (range, 34-54 mm), and the tendon shape is asymmetrical, with a maximum length of 89 mm on average (range, 78-100 mm) typically occurring 62% from the medial border of the QTpatellar insertion. The QT increases in thickness from proximal to distal as aponeurotic layers of the extensor apparatus merge, reaching a mean maximum thickness of 7.9 mm (range, 6.5-9.5 mm) at the distal insertion.7 Hence, QT graft harvesting may be full thickness, partial thickness, or a mixture of both at different distances along the proximal-to-distal axis. Even in cases of full-thickness harvesting, the synovium is often not breached. When one is closing the tendon defect, placement of stitches in the superficial aspect of the tendon is recommended to avoid bunching or shortening of the tendon (fanlike closure).

 Become a member
Become a member