- Home
- Introduction
- Techniques
- Minimally Invasive Harvest Of A Quadriceps Tendon Graft With or Without A Bone Block
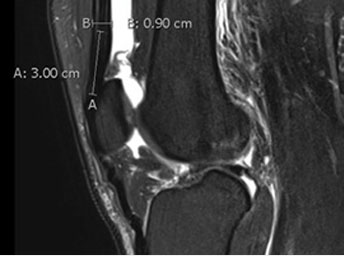
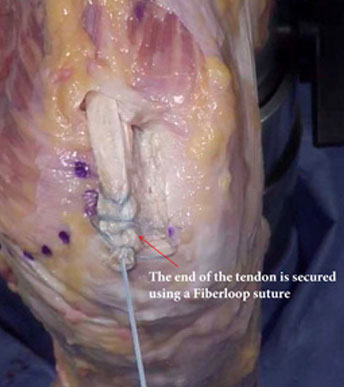
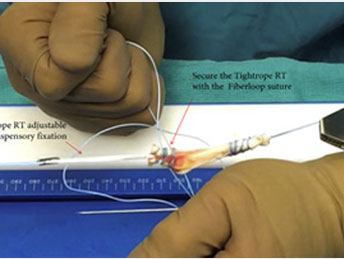
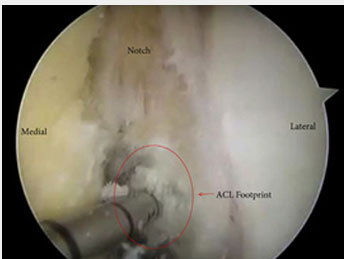
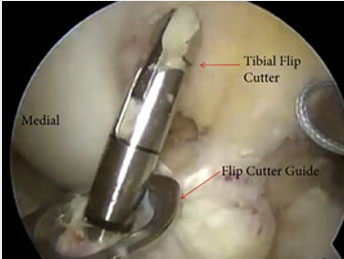
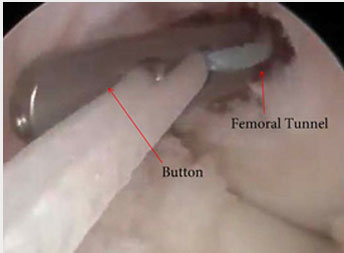
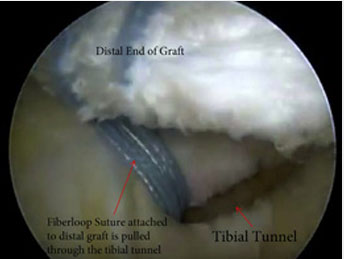
- Minimally Invasive Quadriceps Tendon Harvest And Graft Preparation For All-inside Anterior Cruciate Ligament Reconstruction
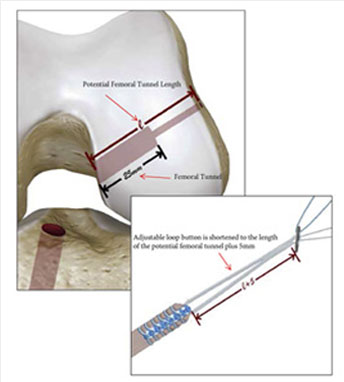
- Minimally Invasive Quadriceps Tendon Single-bundle Arthroscopic, Anatomic Anterior Cruciate Ligament Reconstruction With Rectangular Bone Tunnels
- Members
- Meetings
- Publications
- News
 Become a member
Become a member